

Correct!
4. All of the above
All of the above considerations are appropriate. In particular, CT of the abdomen and pelvis is indicated urgently to exclude abscess, bowel obstruction, and other complications related to inflammatory bowel disease.
The patient did not have a recent travel history, but did live in the Philippines 11 years ago. She was referred for CT examination of the abdomen and pelvis (Figure 1), which showed colitis extending from the distal transverse colon through the rectum.
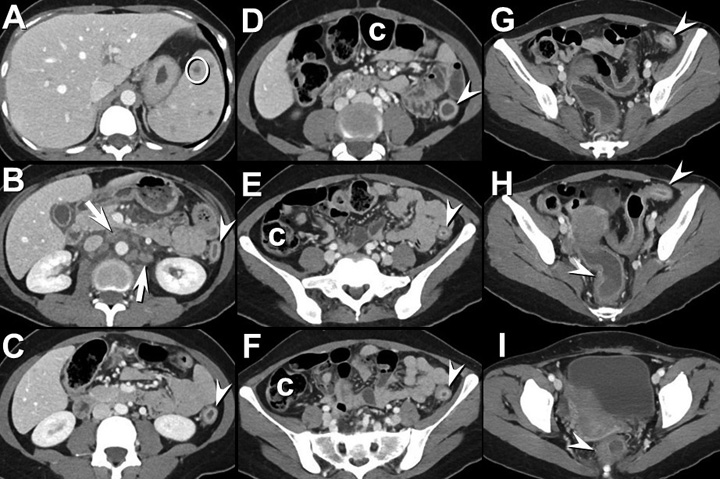
Figure 1. Figure 1A-I: Axial enhanced abdominal CT shows diffuse colonic thickening extending from the distal transverse colon through the rectum (arrowheads) as well as retroperitoneal lymphadenopathy (arrows). Small non-specific hypoattenuating splenic lesions (circle) and nonspecific gallbladder wall thickening are also present. c = normal right and transverse colon; note thin wall. Right: Video of abdominal CT scan.
Additionally, this examination revealed abnormal soft tissue in the porta hepatis and retroperitoneal lymphadenopathy as well as non-specific low attenuation splenic lesions. Gastroenterology (GI) was consulted and recommended testing to exclude gastrointestinal pathogens prior to initiation of intravenous corticosteroids as well as testing for possible SARS-CoV-2 infection. The presence of the lymph node enlargement at CT raised concern for a second, superimposed process, including potential malignancy; GI recommended MR enterography for evaluation of these lymph nodes as well as soft tissue in the porta hepatis and the splenic lesions. Small bilateral basal pulmonary nodules (Figure 2) were incidentally noted as well.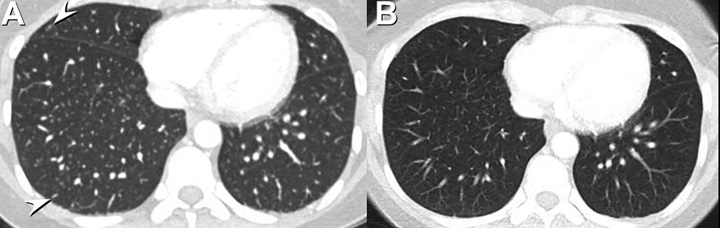
Figure 2. Comparison of lung bases from CT abdomen and pelvis at presentation (A) and 1 month earlier while the patient was hospitalized at an outside institution. Note that numerous, small, circumscribed nodules at presentation (arrowheads, A) have developed over the previous month (B).
The MR enterography study showed the large bowel inflammation, focal splenic lesions, and lymphadenopathy, but nothing of significance in addition to what was already known at CT. Testing for GI pathogens and SARS-CoV-2 was negative, and intravenous corticosteroid therapy was begun. Three sputum acid fast bacillus tests were negative.
Which of the following represents an appropriate next step for the patient’s management? (Click on correct answer to be directed to the third of ten pages)