Court Overturns CMS' Site-Neutral Payment Policy
 Saturday, September 21, 2019 at 8:00AM
Saturday, September 21, 2019 at 8:00AM On Tuesday of this week (9/17/19) a federal district court judge ruled in favor of an American Hospital Association (AHA) and Association of American Medical Colleges (AAMC) complaint that the Centers for Medicare & Medicaid Services (CMS) had overstepped its bounds by implementing site-neutral payments in January. US District Judge Rosemary M. Collyer said in her decision, "The Court finds that CMS exceeded its statutory authority when it cut the payment rate for clinic services at off-campus provider-based clinics" (1).
Under its site-neutral policy, CMS had begun paying the outpatient provider-based departments of hospitals the same for visits that it paid to independent physician practices. Previously, the hospital providers had been paid significantly more for these services than to community practices and the change in CMS policy was expected to level the playing field between independent offices and hospital-employed practices. In addition, it lowered the incentive of healthcare systems to acquire more physicians and their practices, according to some health policy experts.
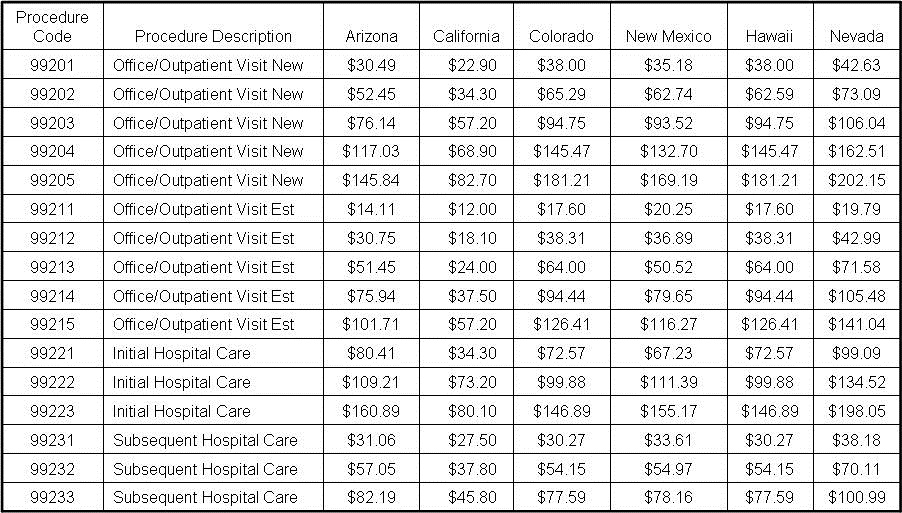
The difference in costs is substantial with hospitals charging 2-6 times more than an independent physician office (2). The site-neutral payments were expected to cost hospitals $760 million in 2020, according to the suit.
The Medicare Payment Advisory Commission had advised Congress that hospitals were buying physician offices and converting them to off-campus provider-based departments partly because payments were higher than independent physician offices. In the Bipartisan Budget Act of 2015, Congress allowed hospitals to bill CMS at the higher outpatient department rate if they existed prior to Nov. 2, 2015. The law permitted CMS to change the payment system for newly established hospital-based outpatient departments. However, one expert told Medscape Medical News last year that this provision of the budget act hadn't had much impact, because many hospitals just added newly recruited physicians to the PBDs that had been grandfathered in (1).
Asked to comment on the court ruling, a CMS spokesperson told Medscape Medical News, "We are aware of the decision and are determining next steps" (1). The AHA and the AAMC were jubilant. In a joint statement, they said, "We are pleased with the District Court's decision that the Department of Health and Human Services exceeded its statutory authority when it reduced payments for hospital outpatient services provided in grandfathered, off-campus, provider-based departments. The ruling, which will allow hospitals to maintain access to important services for patients and communities, affirmed that the cuts directly undercut the clear intent of Congress to protect hospital outpatient departments because of the many real and crucial differences between them and other sites of care."
John Cullen, MD, president of the American Academy of Family Physicians, said in a statement that the AAFP is disappointed with the court ruling. "The decision preserves a system that both costs patients more in out-of-pocket expenses and limits their choice of physicians by paying hospital outpatient departments more for the same services provided by community-based physicians." he said. He added, these payment disparities across sites of service "force many community clinics to close their doors or sell their practices to hospitals. The small private practices, which provide high-quality care at a lower cost, are most at risk as a result of this decision." Robert Doherty, senior vice president, governmental affairs and public policy, for the American College of Physicians, tweeted, "This is very bad news for all the patients harmed by hospitals adding 'facility fees' for visits to doctors in practices they acquired."
Richard A. Robbins, MD
Editor, SWJPCC
References
- Terry K. Court overturns CMS' site-neutral payment policy; doc groups upset. Medscape Medical News. September 19, 2019. Available at: https://www.medscape.com/viewarticle/918744?nlid=131645_5401&src=wnl_dne_190920_mscpedit&uac=9273DT&impID=2101100&faf=1#vp_2 (accessed 9/19/19).
- Carey MJ. Facility fees: the farce everyone pays for. Medical Economics. August 16, 2018. Available at: https://www.medicaleconomics.com/blog/facility-fees-farce-everyone-pays (accessed 9/19/19).
Cite as: Robbins RA. Court overturns CMS' site-neutral payment policy. Southwest J Pulm Crit Care. 2019;19(3):101-2. doi: https://doi.org/10.13175/swjpcc060-19 PDF