CDC Warns of Increased Ivermectin Overdoses
 Friday, August 27, 2021 at 10:12AM
Friday, August 27, 2021 at 10:12AM The US Centers for Disease Control and Prevention (CDC) is warning of an increase in cases of ivermectin overdose due to people self-prescribing the drug in an effort to prevent or treat COVID-19 (1). Ivermectin is used to treat river blindness and intestinal roundworm infection in humans and to de-worm pets and livestock.
A study published earlier this year showed that ivermectin killed SARS-CoV-2 in cells in vitro. The authors proposed that the medication be investigated as a cheap and easily available treatment for COVID-19. However, subsequent studies have failed to find any benefit in humans (3).
In a new communication to its Health Alert Network, the CDC says cases of overdose and misuse are rising (1). More than 88,000 prescriptions were written for the drug ivermectin in the week ending August 13, an increase of 2400% over the weekly average prior to the COVID-19 pandemic (Figure 1).
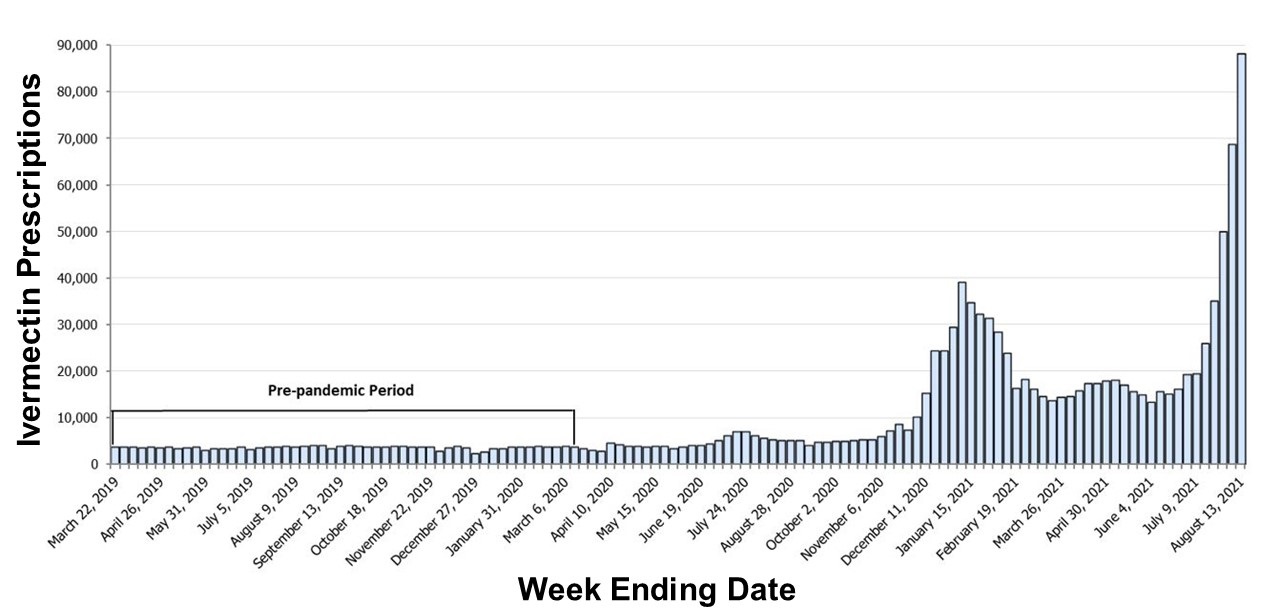
Figure 1. Ivermectin prescriptions by week (from CDC, reference 1).
Unfortunately, the signs of overdose are nonspecific but can include gastrointestinal symptoms (nausea, vomiting, and diarrhea), hypotension and altered mental status (change in consciousness, confusion, hallucinations, seizures, coma).
The CDC is asking doctors to alert their patients to the risks of ivermectin, particularly ivermectin products intended for veterinary use. Physicians might suspect ivermectin in a patient with unexplained symptoms and are encouraged to contact their local poison control for assistance.
References
- CDC. Rapid Increase in Ivermectin Prescriptions and Reports of Severe Illness Associated with Use of Products Containing Ivermectin to Prevent or Treat COVID-19. August 26, 2021. Available at: https://emergency.cdc.gov/han/2021/han00449.asp (accessed 8/27/21).
- Caly L, Druce JD, Catton MG, Jans DA, Wagstaff KM. The FDA-approved drug ivermectin inhibits the replication of SARS-CoV-2 in vitro. Antiviral Res. 2020 Jun;178:104787. [CrossRef] [PubMed]
- Popp M, Stegemann M, Metzendorf MI, Gould S, Kranke P, Meybohm P, Skoetz N, Weibel S. Ivermectin for preventing and treating COVID-19. Cochrane Database Syst Rev. 2021 Jul 28;7:CD015017. [CrossRef] [PubMed]
Cite as: Robbins RA. CDC Warns of Increased Ivermectin Overdoses. Southwest J Pulm Crit Care. 2021;23(2):62-3. doi: https://doi.org/10.13175/swjpcc038-21 PDF
