Medical Image of the Month: Glioblastoma Multiforme
 Wednesday, September 2, 2020 at 8:00AM
Wednesday, September 2, 2020 at 8:00AM 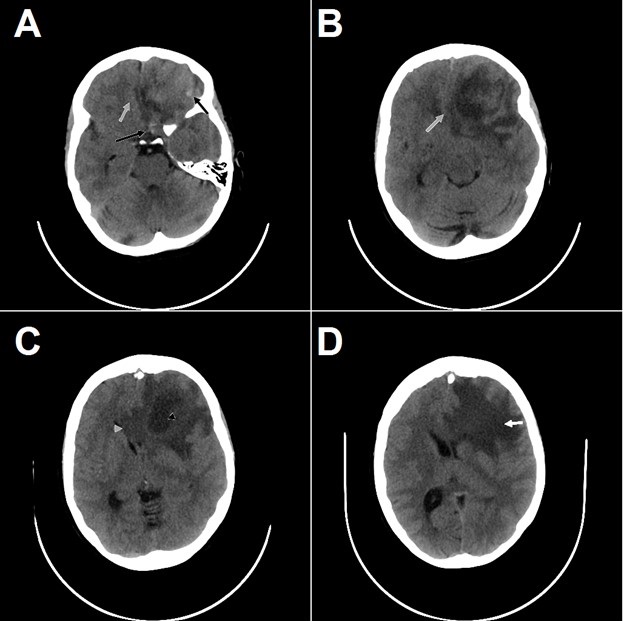
Figure 1. Non-contrast CT axial views of what was later identified as glioblastoma multiforme demonstrates heterogeneous left frontal lobe mass with foci of hemorrhage (black arrows, A), mass effect (gray arrow, A & B), central necrosis (gray arrowhead, C), invasion of the corpus callosum (gray arrowhead, C), and vasogenic edema (white arrow, D).
A patient in their 60's presented with headaches for approximately 2 weeks followed by acutely worsening mental status with confusion. CT of the head is shown (Figure 1). Glioblastoma multiforme was high on the differential diagnosis.
Glioblastoma multiforme (GBM) is classified as a grade IV astrocytoma and is the most common malignant primary brain tumor. It has an incidence of 3.19 cases per 100,000 persons per year. Astrocytomas are the most invasive type of glial tumor, directly reflecting the remarkably poor prognosis with a 5-year survival rate of approximately 4% and a 26-33% survival rate at 2 years in clinical trials. Symptoms develop relatively rapidly due to edema and mass effect of the tumor. Increased intracranial pressure and swelling manifests as nausea, vomiting, seizures and headaches that are typically worse in the morning. Neurological symptoms are dependent on the location of the cerebrum that is affected (ex. sensory, motor, visual changes, gait disturbances). Conventional gadolinium-enhanced MR imaging is the standard technique for the evaluation of GBM. GBM is characterized by a large, heterogeneous mass in the cerebral hemisphere exhibiting hemorrhage, necrosis and enhancement. In addition, magnetic resonance tomography (MRS) and positron emission tomography (PET) can be used to examine the chemical profile and assist in detecting tumor recurrence, respectively. The current gold standard treatment for GBM is temozolomide in combination with radiation therapy. Two potential new treatment modalities currently under investigation are gene therapy and immunotherapy.
Biopsy of the patient’s mass confirmed glioblastoma multiforme, which was successfully treated without recurrence on MRI 18 months later.
Cassandra Ann Roose and Michael Craig Larson MD, PhD
Medical Imaging Department
Banner University Medical Center/University of Arizona
Tucson, AZ UA
References
- Stoyanov GS, Dzhenkov DL. On the Concepts and History of Glioblastoma Multiforme - Morphology, Genetics and Epigenetics. Folia Med (Plovdiv). 2018;60(1):48-66. [CrossRef] [PubMed]
- Altman DA, Atkinson DS Jr, Brat DJ. Best cases from the AFIP: glioblastoma multiforme. Radiographics. 2007;27(3):883-888. [CrossRef] [PubMed]
- American Association of Neurological Surgeons. Glioblastoma Multiforme. Available from: https://www.aans.org/en/Patients/Neurosurgical-Conditions-and-Treatments/Glioblastoma-Multiforme (accessed 8/24/20).
Cite as: Roose CA, Larson MC. Medical image of the month: glioblastoma multiforme. Southwest J Pulm Crit Care. 2020;21(3):64-5. doi: https://doi.org/10.13175/swjpcc046-20 PDF

Reader Comments (1)
Wow, this case is both fascinating and terrifying. GBM is already known to be aggressive, but seeing those CT details—hemorrhage, necrosis, edema, even the corpus callosum involvement—really shows how quickly it can take over. It’s honestly amazing the patient had such a good outcome, especially with no recurrence on MRI after 18 months. Huge respect to the team at Banner/University of Arizona for highlighting how important fast diagnosis and treatment are with something this serious.