Fake News in Healthcare
 Friday, October 27, 2017 at 8:00AM
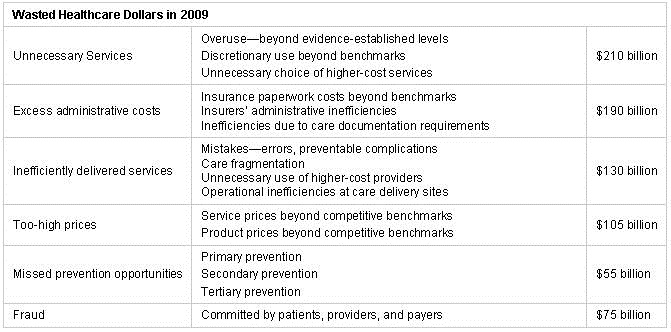
Friday, October 27, 2017 at 8:00AM An article in the National Review by Pascal-Emmanuel Gobry points out that there is considerable waste in healthcare spending (1). He blames much of this on two entitlements-Medicare and employer-sponsored health insurance. He also lays much of the blame on doctors. “Doctors are the biggest villains in American health care. ... As with public-school teachers, we should be able to recognize that a profession as a whole can be pathological even as many individual members are perfectly good actors, and even if many of them are heroes. And just like public-school teachers, the medical profession as a whole puts its own interests ahead of those of the citizens it claims to be dedicated to serve.”
Who is Pascal-Emmanuel Gobry and how could he say something so nasty about teachers and my profession? A quick internet search revealed that Mr. Gobry is a fellow at the Ethics & Public Policy Center, a conservative Washington, D.C.-based think tank and advocacy group (2). According to his biography, Gobry writes about religion, culture, politics, economics, business, and technology, but not health care. He is a columnist at The Week, a contributor at Forbes, a blogger at the Patheos Catholic and his writing has appeared in the Wall Street Journal, The Atlantic, and The Daily Beast amongst others. He holds a Master of Science in management from HEC Paris (Hautes études commerciales de Paris, a quite prestigious business school) and lives in Paris.
To make his point on waste, Mr. Gobry comments on Atul Gawande’s 2007 New Yorker “exposé on the Herculean efforts by a handful of scientists to get intensive-care physicians to implement a basic hygiene measures checklist so as to stop hospital-borne diseases” (3). He goes on to quote the Centers for Disease Control that hospital-borne diseases kill about 100,000 people per year, that the checklist was of no cost to the doctors, and its scientific rationale was unquestionable. “Doctors still resisted it with all their might because they found it mildly inconvenient; perhaps they found it even less acceptable that anybody might tell them how to do their jobs”. I showed this article to one of my former pulmonary/critical care fellows who has been in practice about 10 years. He commented, “Another guy who doesn’t practice medicine or know what he’s talking about.”
Gobry is referring to the Institute of Healthcare Improvement (IHI) central line associated blood stream infection (CLABSI) guidelines. These include hand washing, sterile gloves, sterile gown, wearing of a cap, full body drape, chlorhexidine, and not using femoral sites for insertion. In our intensive care units only chlorhexidine usage was associated with a decline in CLABSI (4). Every ICU I have practiced in has emphasized handwashing and demanded use of sterile gloves, gowns and drapes. The remaining guidelines are not supported by good evidence.
Gobry also claims that a computer is better at diagnosis than most physicians. He claims that the evidence is “pretty robust at this point, and the profession resists it tooth and nail. In a few years, we’ll be able to know how many unnecessary deaths this led to, but the number will have lots of zeroes”. However, in the only direct comparison of diagnostic accuracy, physicians vastly outperformed computer algorithms (84.3% vs. 51.2%) (5).
Journalists like Gobry are writing melodramatic articles about medicine and often getting it wrong. In this case he sensationalized Gawande’s article and misquoted the evidence for both the IHI guidelines and computer diagnosis.
There’s a TV commercial about an actor playing a doctor. Gobry is a business journalist attempting to play a doctor at the National Review. My former fellow is right. Gobry is a guy who does not know what he is talking about. Unfortunately, his writings can affect public policy and influence politicians who know even less. As President Trump said, “Nobody knew that health care could be so complicated” (6).
I am a doctor playing a journalist at the Southwest Journal of Pulmonary and Critical Care. Our articles may not be as sensational as Gobry’s, but we stick to what we know-pulmonary, critical care and sleep medicine. I think we usually get it right. President Trump has railed against “fake news”, most recently on Lou Dobbs Tonight (7). Journalists like Gobry contribute to fake news by being deliberately obtuse, appealing to emotions, name-calling, and omitting or distorting facts. As physicians, we have been denigrated by journalists like Gobry and others who make outrageous claims for their own purposes. It is the responsibility of physicians to challenge those like Gobry who get it wrong.
Richard A. Robbins, MD
Editor, SWJPCC
References
- Gobry P-E. The most wasteful health spending is also the most popular. National Review. October 25, 2017. Available at: http://www.nationalreview.com/article/453088/health-care-spending-wasteful-popular (accessed 10/25/17).
- Ethics & Public Policy Center. Pascal-Emmanuel Gobry. https://eppc.org/author/pascal-emmanuel-gobry/ (accessed 10/25/17).
- Gawande A. The Checklist. The New Yorker. December 10, 2007. Available at: https://www.newyorker.com/magazine/2007/12/10/the-checklist (accessed 10/25/17).
- Hurley J, Garciaorr R, Luedy H, et al. Correlation of compliance with central line associated blood stream infection guidelines and outcomes: a review of the evidence. Southwest J Pulm Crit Care 2012;4:163-73. Available at: http://www.swjpcc.com/critical-care/2012/5/10/correlation-of-compliance-with-central-line-associated-blood.html.
- Semigran HL, Levine DM, Nundy S, Mehrotra A. Comparison of Physician and Computer Diagnostic Accuracy. JAMA Intern Med. 2016 Dec 1;176(12):1860-1861. [CrossRef] [PubMed]
- Howell T Jr. Trump: 'Nobody Knew That Health Care Could Be So Complicated'. Fox News. February 27, 2017. Available at: http://nation.foxnews.com/2017/02/27/trump-nobody-knew-health-care-could-be-so-complicated (accessed 10/25/17).
- Trump DJ. Lou Dobbs Tonight. October 25, 2017. Available at: http://video.foxbusiness.com/v/5624925494001/?#sp=show-clips (accessed 10/26/17).
Cite as: Robbins RA. Fake news in healthcare. Southwest J Pulm Crit Care. 2017;15(4):171-3. doi: https://doi.org/10.13175/swjpcc132-17 PDF