Pediculosis As a Possible Contributor to Community-Acquired MRSA Bacteremia and Native Mitral Valve Endocarditis
 Wednesday, May 4, 2022 at 8:00AM
Wednesday, May 4, 2022 at 8:00AM Ali A. Mahdi MD, Charis Tjoeng DO, Vishal Patel MD, Serap Sobnosky MD
Dignity Health St Mary Medical Center
Department of Internal Medicine
Long Beach, California USA
Abstract
Methicillin-resistant Staphylococcus aureus (MRSA) bacteremia is a known cause of infective endocarditis. In this case report, we describe a patient with community-acquired MRSA bacteremia and subsequent mitral valve endocarditis. This patient was noted to be without commonly recognized risk factors for MRSA bacteremia, thus her likely source was skin colonization, with skin trauma facilitated by pediculosis infestation.
Case Presentation
An elderly woman was brought to the Emergency Department after being found down. A bystander called EMS after finding her lying on the ground next to a pool of emesis. Per EMS, the patient was found to have pinpoint pupils with Glasgow Coma Scale (GCS) 4-1-4, with only minimal improvement with a dose of naloxone. After admission she was noted to be afebrile, with a III/VI systolic murmur and an extensive infestation of lice in her hair. Urine toxicology screen was negative. CT radiography of her head was negative for acute intracranial pathology, with chronic ischemic changes. Blood cultures were drawn from two peripheral sites, but as the patient was afebrile without leukocytosis, she was not started on antibiotics. Her identity was later confirmed, and she was noted to be 72 years old with a history of homelessness. She had previously denied a history of IV drug abuse or previous surgeries, and was not noted to be hospitalized recently.
On the second day of hospitalization, her mentation improved, and she was described as coherent on exam. However, she became febrile to maximum temperature 38.5° C with a new leukocytosis to 14,500. Two of two blood cultures, drawn on admission, resulted in gram positive cocci with clusters, and she was started on empiric vancomycin therapy. The initial two blood cultures, as well as two repeat blood cultures later speciated to methicillin-resistant Staphylococcus aureus (MRSA). MRSA nares swab results were negative. However, as the patient was noted to have persistent pediculosis infestation, a possible source of MRSA bacteremia was skin colonization introduced to her bloodstream through excoriations. An infectious disease specialist was consulted, who recommended a transthoracic as well as a transesophageal echocardiogram.
Transthoracic echocardiography (TTE) revealed a moderate mobile vegetation on the posterior mitral valve leaflet (Figure 1A), as well as severe mitral regurgitation (Figure 1B).
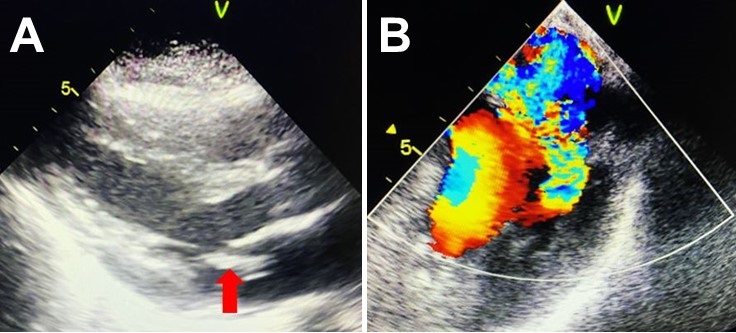
Figure 1. Transthoracic echocardiography showing large vegetation on posterior leaflet of mitral valve (A) and severe mitral regurgitation resulting from large vegetation (B).
Left ventricular ejection fraction was reported to be 55-60%, with no other vegetations noted. On day five of hospitalization, the patient underwent transesophageal echocardiography (TEE), which revealed large vegetation on the posterior leaflet measuring 2.5 x 0.8 cm (Figure 3) causing severe mitral regurgitation (Figure 2).
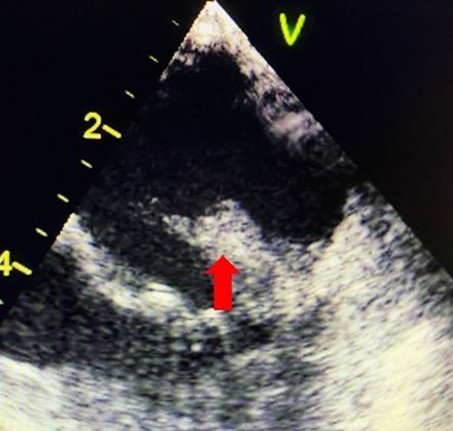
Figure 2. Transesophageal echocardiography redemonstrating large vegetation on mitral valve (red arrow), measuring 2.5 x 0.8 cm.
A cardiothoracic surgery evaluation was obtained for mitral valve replacement, and she was deemed a surgical candidate.
In preparation for surgical intervention, cardiac catheterization was performed, which revealed no coronary artery disease. The patient’s pediculosis was noted to persist despite three topical treatments and two doses of oral ivermectin, and an additional dose of ivermectin was planned. Two repeat blood cultures resulted in no growth, and the patient was pending cardiothoracic surgery. However, on the day of surgery, the patient elected to leave against medical advice (AMA) despite extensive counseling. She had received 18 days total of IV vancomycin.
Discussion
MRSA continues to cause significant morbidity and mortality both in healthcare and community populations. S. aureus bacteremia can often cause complications, most concerning infective endocarditis, osteomyelitis, and sepsis. Incidence of community-acquired MRSA bacteremia, including healthcare-associated cases, has increased in recent years, surpassing rates of hospital-acquired infections globally (1-3). MRSA colonization increases the risk of MRSA infections and bacteremia; in a study of 29371 hospitalized patients, MRSA-colonized (per nasal swab) patients were 19.89 times more likely to develop bacteremia than non-colonized patients (4). Sites of S. aureus colonization include the nares, nasopharynx, skin, wound sites, and vascular catheters. Once colonized, traumatic injury or disruption can facilitate invasion of S. aureus into deeper structures of the skin, which can in turn lead to bacteremia.
There have been no documented cases of pediculosis as a contributor to MRSA bacteremia. However, lice have been identified as vectors for several pathogens, including Bartonella quintana, Rickettsia prowazekii, and Borrelia recurrentis (5). In particular, pediculosis has been shown to be associated with B. quintana seroconversion and bacteremia in a study of homeless individuals (6). B. quintana,is a gram negative bacteria transmitted by responsible for trench fever in World War I, during which it was transmitted by lice. More recently, it has been reported to cause bacillary angiomatosis, acute and chronic bacteremia, and endocarditis, with homeless persons and individuals with alcoholism at significant risk (7). Bartonella species including B. quintana have recently been described as emerging causes of culture-negative endocarditis (8). Notably, one case report documents a patient with a history of pediculosis, found to have culture-negative endocarditis. TEE revealed a 2.5 x 0.9 cm vegetation on the mitral valve and several small vegetations on the aortic valve. Serology was positive for both B. quintana and B. henselae, and rRNA sequencing confirmed B. quintana infection of both valves (9).
On TEE, our patient was shown to have a large vegetation on the mitral valve, measuring 2.5 x 0.8 cm in diameter. Given the high risk of embolization and severe mitral, valve replacement surgery was highly recommended. Per ID specialist, a six-week course of antibiotics was also recommended for complicated bacteremia. Unfortunately, the patient left against medical advice (AMA) before surgical intervention and before an appropriate duration of antibiotics.
The source of this patient’s bacteremia was initially unclear, as she did not have common risk factors for MRSA bacteremia. She denied IV drug use, was not recently admitted to a hospital or nursing facility, did not have any chronic conditions or prosthetic devices, and was found to have a negative MRSA nares swab. Thus, her source of infection was possibly skin colonization with MRSA, with introduction into her bloodstream facilitated by excoriations due to persistent pediculosis infestation. She was noted to have a significant amount of lice despite several topical and oral medications, and left AMA before completing a three-dose course of ivermectin.
Conclusion
In this case report, we describe a patient with community-acquired MRSA bacteremia and subsequent mitral valve endocarditis. In the absence of common risk factors, her likely source of infection was considered to be skin colonization, with skin barrier disruption from excoriations due to pediculosis.
References
- Gould IM, David MZ, Esposito S, Garau J, Lina G, Mazzei T, Peters G. New insights into meticillin-resistant Staphylococcus aureus (MRSA) pathogenesis, treatment and resistance. Int J Antimicrob Agents. 2012 Feb;39(2):96-104. [CrossRef] [PubMed]
- Turner NA, Sharma-Kuinkel BK, Maskarinec SA, Eichenberger EM, Shah PP, Carugati M, Holland TL, Fowler VG Jr. Methicillin-resistant Staphylococcus aureus: an overview of basic and clinical research. Nat Rev Microbiol. 2019 Apr;17(4):203-218. [CrossRef] [PubMed]
- Hassoun A, Linden PK, Friedman B. Incidence, prevalence, and management of MRSA bacteremia across patient populations-a review of recent developments in MRSA management and treatment. Crit Care. 2017 Aug 14;21(1):211. [CrossRef] [PubMed]
- Marzec NS, Bessesen MT. Risk and outcomes of methicillin-resistant Staphylococcus aureus (MRSA) bacteremia among patients admitted with and without MRSA nares colonization. Am J Infect Control. 2016 Apr 1;44(4):405-8. [CrossRef] [PubMed]
- Brouqui P, Lascola B, Roux V, Raoult D. Chronic Bartonella quintana bacteremia in homeless patients. N Engl J Med. 1999 Jan 21;340(3):184-9. [CrossRef] [PubMed]
- Brouqui P, Stein A, Dupont HT, Gallian P, Badiaga S, Rolain JM, Mege JL, La Scola B, Berbis P, Raoult D. Ectoparasitism and vector-borne diseases in 930 homeless people from Marseilles. Medicine (Baltimore). 2005 Jan;84(1):61-68. [CrossRef] [PubMed]
- Spach DH, Kanter AS, Dougherty MJ, Larson AM, Coyle MB, Brenner DJ, Swaminathan B, Matar GM, Welch DF, Root RK, et al. Bartonella (Rochalimaea) quintana bacteremia in inner-city patients with chronic alcoholism. N Engl J Med. 1995 Feb 16;332(7):424-8. [CrossRef] [PubMed]
- Okaro U, Addisu A, Casanas B, Anderson B. Bartonella Species, an Emerging Cause of Blood-Culture-Negative Endocarditis. Clin Microbiol Rev. 2017 Jul;30(3):709-746. [CrossRef] [PubMed]
- Boodman C, Wuerz T, Lagacé-Wiens P. Endocarditis due to Bartonella quintana, the etiological agent of trench fever. CMAJ. 2020 Dec 7;192(49):E1723-E1726. [CrossRef] [PubMed]

Reader Comments