A Case and Brief Review of Bilious Ascites and Abdominal Compartment Syndrome from Pancreatitis-Induced Post-Roux-En-Y Gastric Remnant Leak
 Sunday, July 11, 2021 at 8:00AM
Sunday, July 11, 2021 at 8:00AM Marissa A. Martin, MD1
Michael H. Lee, MD2
Anna Neumeier, MD3
Tristan J. Huie, MD3
1 University of Colorado Department of Internal Medicine
2 University of California, San Francisco Division of Pulmonary and Critical Care Medicine
3 University of Colorado Division of Pulmonary Sciences and Critical Care Medicine
Abstract
This is a case of a 55-year-old man with Roux-en-Y gastric bypass surgery 15 years prior who presented with acute pancreatitis and developed distributive shock, bacteremia, acute respiratory distress syndrome, anuric acute renal failure, and a distended abdomen with increasing ascitic fluid on imaging. An elevated bladder pressure, lactic acidosis, and anuria raised concern for abdominal compartment syndrome. Paracentesis was done and four liters of bilious ascitic fluid were drained. Intra-abdominal pressure was measured and improved from 27 cmH2O to 13 cmH2O with paracentesis. Mean arterial pressure and urine output also improved. The patient developed recurrent loculated intra-abdominal fluid collections, though ultrasound, CT scans with and without contrast, MRCP, ERCP, upper GI fluoroscopy, and small bowel enteroscopy failed to reveal a source of the bilious output. Ultimately, a gastrostomy tube was placed and delivery of contrast material through the tube revealed active extravasation from the remnant stomach. This case underscores the importance of considering post-surgical leak regardless of how remotely a Roux-en-Y surgery took place, confirms the importance of pursuing early gastrostomy tube placement and contrast administration when post-Roux-en-Y gastric remnant leaks are suspected, and demonstrates the role of paracentesis in critically ill patients with abdominal compartment syndrome.
Background
Post-surgical leaks complicate up to 7% of Roux-en-Y gastric bypass procedures and they result in greater than 50% morbidity and mortality (1,2). Most leaks (between 69% and 77%) occur at the gastrojejunal anastomosis, and on average, they become symptomatic three days after surgery (3,4). Rare leaks from the gastric remnant, which is the larger portion of the stomach that during a Roux-en-Y surgery is bypassed with the gastrojejunal anastomosis, have been reported and have been said to have delayed presentations, though this has typically only been weeks after surgery, not years (1,5). This is a case of post-Roux-en-Y gastric remnant leak that occurred 15 years after the original surgery, underscoring the importance of considering post-surgical leak as a diagnostic possibility regardless of how remotely a Roux-en-Y surgery took place. This case discusses a possible provoking factor, illustrates the clinical presentation, and suggests a diagnostic and treatment approach for these leaks. As morbid obesity becomes more prevalent in today’s society and Roux-en-Y gastric bypass procedures become even more mainstream, knowledge of delayed complications, such as the one discussed in this case, is crucial.
Case Report
A 55-year-old man with a past medical history of atrial fibrillation, previous alcohol-induced acute pancreatitis, and Roux-en-Y gastric bypass surgery 15 years prior presented with three days of abdominal pain and pre-syncope. He was drinking four to five alcoholic drinks daily. On presentation to the emergency department, the patient was in atrial fibrillation with a heart rate greater than 160 beats/min and was hypotensive to 77/53 mmHg. He was afebrile and mildly leukopenic with a white blood cell count of 4.4 k/mL. He had a lactate level of 12.5 mmol/L and a lipase of 1756 U/L with clinical and radiographic evidence of acute pancreatitis (Figure 1).
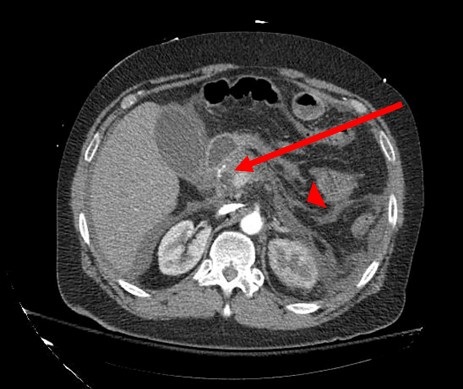
Figure 1. CT scan showing an enlarged pancreatic head and proximal body (arrow) with peripancreatic fat stranding (arrowhead), consistent with acute pancreatitis.
He was admitted to the medical intensive care unit, where over the next two days his distributive shock was complicated by Enterobacter cloacae bacteremia, acute respiratory distress syndrome, and acute anuric renal failure. For the management of his multi-organ failure, the patient was placed on mechanical ventilation, paralytic therapy, and infusions of norepinephrine, vasopressin, and phenylephrine. He was also started on continuous renal replacement therapy.
On hospital day three, the patient developed increasing abdominal distention with CT showing an interval increase in the size of ascites. An elevated bladder pressure of 21 mmHg, measured following the administration of rocuronium, along with a lactate of 12.3 mmol/L and anuria raised the concern for abdominal compartment syndrome. Paracentesis was done and four liters of bilious ascitic fluid were drained (Figure 2).
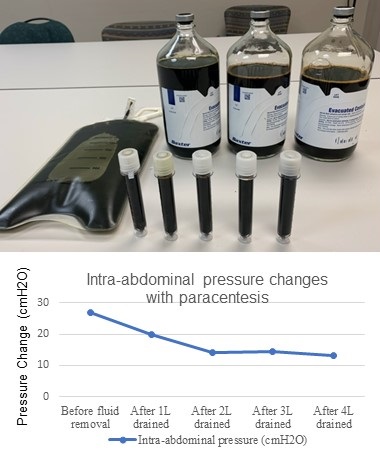
Figure 2. Paracentesis drained four liters of bilious fluid. Using a manometer, intra-abdominal pressure was measured first prior to fluid removal and subsequently after each liter was drained. The intra-abdominal pressure was 27 cmH2O initially and decreased to 13 cmH2O.
Using the manometer from a lumbar puncture kit, intra-abdominal pressure was measured first prior to fluid removal and subsequently after each liter was drained. With fluid removal, the initial intra-abdominal pressure of 27 cmH2O improved to 13 cmH2O (Figure 2), and the mean arterial pressure increased by 16 mmHg (from 70 mmHg to 86 mmHg). The norepinephrine, which had been infusing at 0.1 mcg/kg/min, was discontinued over the subsequent hour and a half, and the patient maintained a mean arterial pressure of 85 mmHg. Over the subsequent 12 hours, the patient’s urine output increased, and continuous renal replacement therapy was discontinued. Analysis of the ascitic fluid showed significantly elevated total bilirubin (17 mg/dL), lactate dehydrogenase (3545 U/L), and amylase (1481 U/L). Serum ascites albumin gradient was 1.1.
Over the next two weeks, the patient developed recurrent loculated intra-abdominal fluid collections (Figure 3) and leukocytosis (as high as 31.9 k/mL) refractory to two additional paracenteses with large volume ascitic fluid removal and broad-spectrum antibiotic treatment.
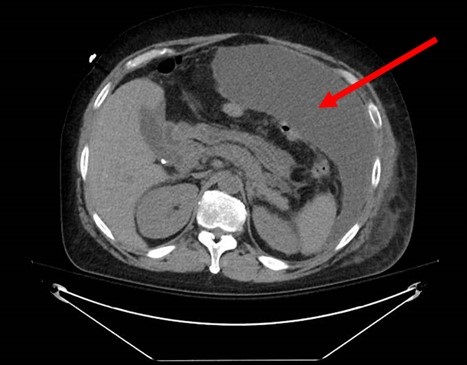
Figure 3. CT scan showing recurrent loculated intra-abdominal fluid collections (arrow) despite broad spectrum antibiotics and repeated paracenteses.
For definitive management of the recurrent ascites, two intra-abdominal drains were placed with fluid cultures growing Candida albicans. Intravenous micafungin was started, which was later narrowed to oral fluconazole. Continued high bilious output from the drains (as high as 3 L daily) raised the suspicion for biliary perforation or a post-Roux-en-Y leak. Multiple imaging studies including ultrasound, CT scans with and without contrast, and magnetic resonance cholangiopancreatography (MRCP), however, did not reveal a source of the bilious output. Although a hepatobiliary iminodiacetic acid (HIDA) scan showed a large leakage at the gastrojejunal anastomotic site, subsequent endoscopic retrograde cholangiopancreatography (ERCP), upper GI fluoroscopy, and small bowel enteroscopy did not demonstrate an overt contrast leak. Ultimately, a gastrostomy tube was placed by interventional radiology and delivery of contrast material through the tube revealed an active extravasation from the remnant stomach (Figure 4).
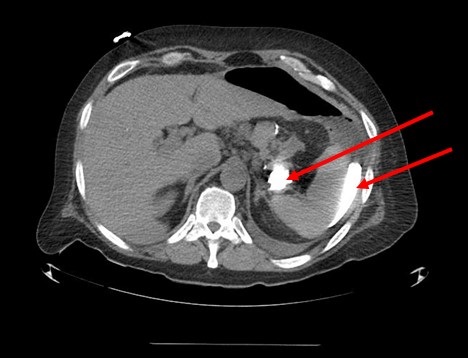
Figure 4. CT scan showing extravasated contrast material (arrows) from the patient’s remnant stomach.
The patient was eventually discharged home on hospital day 28 with one remaining intra-abdominal drain in addition to the gastric tube to allow for gastric decompression and spontaneous healing of the post-Roux-en-Y leak.
Discussion
As discussed in the introduction, post-surgical leaks are a known complication of Roux-en-Y gastric bypass procedures and they have great morbidity and mortality. They most commonly occur at the gastrojejunal anastomosis and are typically detected within days of the original surgery. In our patient, it is likely that his alcohol-induced acute pancreatitis triggered the release of activated proteolytic pancreatic enzymes, which resulted in the gastric remnant leak and infected bilious ascites, a pathophysiologic mechanism previously suggested by one case series (6). Our patient’s delayed presentation 15 years after his Roux-en-Y gastric bypass surgery underscores the importance of considering post-surgical leak as a diagnostic possibility regardless of how remotely the surgery took place.
Diagnosing post-Roux-en-Y gastric remnant leaks can remain challenging even when they are suspected. Our patient’s gastric remnant leak was identified only after contrast delivery through the gastrostomy tube; previous diagnostic studies, including ultrasound, CT scans with and without contrast, MRCP, ERCP, upper GI fluoroscopy, and small bowel enteroscopy were all non-diagnostic. Similar diagnostic difficulty was described in another case of gastric remnant leak also complicated by the formation of amylase-containing dark ascitic fluid, in which the correct diagnosis was made only with CT-guided percutaneous gastrostomy followed by administration of contrast material (5). We hypothesize that this diagnostic difficulty is due to the inability of enteral contrast to reach the decompressed gastric remnant in adequate volume to detect a perforation, since it would be required to move against the typical flow of gastric secretions after a Roux-en-Y procedure. Our case confirms the importance of pursuing early gastrostomy tube placement and contrast administration when post-Roux-en-Y gastric remnant leak is suspected in order to allow for definitive diagnosis and appropriate treatment.
This case also highlights the diagnostic utility of paracentesis in abdominal hypertension or abdominal compartment syndrome, defined as an intra-abdominal pressure ≥ 12 mmHg or an intra-abdominal pressure > 20 mmHg with new organ dysfunction, respectively (7). Although our patient’s distended abdomen, elevated bladder pressure, and anuria collectively raised the concern for abdominal compartment syndrome, his abdomen remained soft. We therefore pursued paracentesis rather than exploratory laparotomy to both achieve an accurate assessment of the intra-abdominal pressure and drain the ascitic fluid. Our patient’s initial intra-abdominal pressure was 27 cmH2O (equivalent to 20 mmHg, similar to the patient’s paralyzed bladder pressure of 21 mmHg), which decreased to 13 cmH2O (or 9.6 mmHg) after four liters of fluid were removed. There was also clear evidence of improvement in end-organ perfusion and function after the paracentesis. We demonstrated a diagnostic as well as therapeutic role of paracentesis in critically ill patients with abdominal compartment syndrome. We showed that paracentesis is a viable alternative to surgical laparotomy, particularly when objective data such as bladder pressure does not correspond with physical examination findings.
References
- Strobos E, Bonanni F. Asymptomatic gastric remnant leak after laparoscopic Roux-en-Y gastric bypass. Surg Obes Relat Dis. 2009 Sep-Oct;5(5):630-2. [CrossRef] [PubMed]
- Madan AK, Lanier B, Tichansky DS. Laparoscopic repair of gastrointestinal leaks after laparoscopic gastric bypass. Am Surg. 2006 Jul;72(7):586-90; discussion 590-1. [PubMed]
- Levine MS, Carucci LR. Imaging of bariatric surgery: normal anatomy and postoperative complications. Radiology. 2014 Feb;270(2):327-41. [CrossRef] [PubMed]
- Lim R, Beekley A, Johnson DC, Davis KA. Early and late complications of bariatric operation. Trauma Surg Acute Care Open. 2018 Oct 9;3(1):e000219. [CrossRef] [PubMed]
- Karmali S, Azer N, Sherman V, Birch DW. Computed tomography-guided percutaneous gastrostomy for management of gastric remnant leak after Roux-en-Y gastric bypass. Surg Obes Relat Dis. 2011 Mar-Apr;7(2):227-31. [CrossRef] [PubMed]
- Schein M, Saadia R, Decker GA. Postoperative pancreatitis--a cause of anastomotic leaks? A report of 4 cases. S Afr Med J. 1988 May 7;73(9):550-1. [PubMed]
- Kirkpatrick AW, Roberts DJ, De Waele J, et al. Intra-abdominal hypertension and the abdominal compartment syndrome: updated consensus definitions and clinical practice guidelines from the World Society of the Abdominal Compartment Syndrome. Intensive Care Med. 2013 Jul;39(7):1190-206. [CrossRef] [PubMed]
Cite as: Martin MA, Lee MH, Neumeier A, Huie TJ. A case and brief review of bilious ascites and abdominal compartment syndrome from pancreatitis-induced post-Roux-en-Y gastric remnant leak. Southwest J Pulm Crit Care. 2021;23(1):18-22. doi: https://doi.org/10.13175/swpcc018-21 PDF

Reader Comments