

Correct!
4. Unable to determine
A hyperechoic area is seen with the right main pulmonary artery (Figure 1).
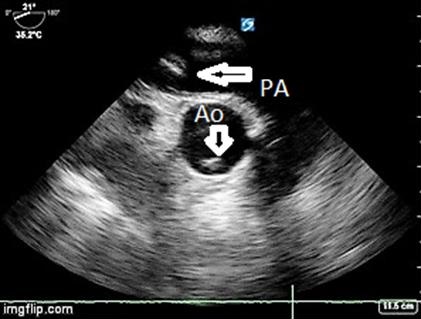
Figure 1. Upper esophageal long-axis view of the pulmonary artery. The pulmonary artery (PA) and Ascending Aorta are labeled (Ao). The left pointing arrow is at a hyperechoic area seen within the right main pulmonary artery concerning for clot. The down-pointing arrow notes an incidental reverberation artifact in the aorta.
Although this is suspicious for pulmonary embolus, the echocardiographer was concerned that this could be an artifact due to reverberation, side lobe artifact or near-field clutter (1). Additionally, the absence of right ventricular dilatation on the 4-chamber view made the echocardiographer more suspicious that this echogenicity might not represent a true finding. More views were obtained with color Doppler in an attempt to determine if flow went around the hyperechoic area, as would be consistent with a clot (Videos 4 and 5).
Video 4. Upper esophageal long-axis view of the pulmonary artery and short axis view of the ascending aorta with color Doppler.
Viewing the videos, the Doppler signal seems to go through the hyperechoic area (suggesting artifact), although this is not clearly definitive. An off-axis view was obtained that appeared to demonstrate that the hyperechoic structure went beyond the walls of the pulmonary artery (Video 6).
Video 6. Upper esophageal oblique view of the pulmonary artery. Artifact traversing the wall of the pulmonary artery.
Given the uncertain nature of the patient’s decompensation, a computerized tomographic angiogram of the chest was performed. It demonstrated a pneumothorax and atelectasis, but no filling defects were seen in the pulmonary artery (Figure 2).

Figure 2. Representative image from CT angiogram of the main pulmonary arteries, demonstrating an absence of a filling defect, at a similar level as the TEE view was obtained.
Ultimately it was determined that the patient’s cardiac arrest was due to a primary respiratory arrest caused by asthma and pneumonia. This potentially misleading artifact in TEE has been demonstrated before (2). The case emphasizes the importance of being aware of imaging artifacts when interpreting ultrasound studies.
References