

Correct!
5. Frontal chest radiography shows rib fractures
The frontal and lateral chest radiographs show mildly displaced left postero-lateral rib fractures associated with soft tissue along the internal aspect of the infero-lateral left chest wall, consistent with pleural effusion or thickening, or possibly extrapleural hematoma, given the rib fractures (Figure 2).
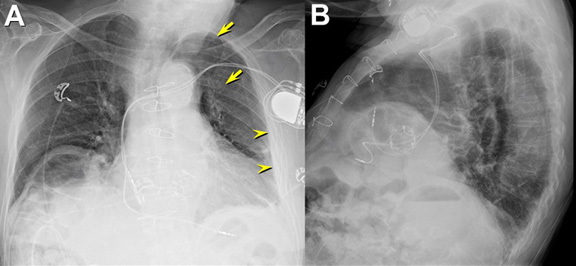
Figure 2. Frontal (A) and lateral (B) chest radiography shows mild cardiomegaly associated with an elevated right diaphragm with a left subclavian pacemaker with leads projected in the right atrial appendage and right ventricle as well as transcatheter aortic valve implantation (Edwards-Sapien, #26). The patient is rotated towards his left (right anterior oblique). A small amount of soft tissue along the left chest wall, which may reflect pleural effusion or pleural thickening (arrowheads), is present. Left postero-lateral rib fractures are seen (arrows).
There is some basal linear opacity consistent with atelectasis, but no focal consolidation to suggest pneumonia, either community-acquired or aspiration-related, is seen, and no cavitary lung mass is evident. No interlobular septal thickening to suggest increased pressure edema is present. The left subclavian pacemaker leads appropriately project in the right atrial appendage and right ventricle, and the transcatheter aortic valve implant appears normally positioned.
Further questioning of the patient’s relatives indicated that he was taking opiates for chest pain related to a left chest wall injury that occurred 15 days earlier, diagnosed at an outside facility, after the patient fell on a rock. It was thought that the patient’s altered mental status may the result of his electrolyte abnormalities in combination with his opiate use. His digoxin level was found to be elevated (3.4 ng/mL, normal = 0.8 – 2 ng/mL, toxic >2.5 ng/mL), but this level was also trended downward after doses were withheld. Head CT was performed, which showed no acute abnormalities. On the second day of his admission, while his delirium persisted, his serum sodium had improved (132 mEq/L; normal = 136 – 145 mEq/L) and his white blood cell count decreased as well. Echocardiography showed a left ventricular ejection fraction of 54% with normal right ventricular function. The aortic valve prosthesis appeared normal positioned with an aortic valve gradient of 6 mmHg.
A blood culture was positive for Streptococcus, thought to reflect bacteremia from the urinary tract infection and previous episodes of self-catheterization. A urinalysis suggested possible urinary tract infection, for which ceftriaxone therapy was begun, and later penicillin was added.
The possibility of infective endocarditis was considered, for which transesophageal echocardiography was performed. This examination showed normal biventricular function, the aortic valve prosthesis appeared normal positioned with an aortic valve gradient of 4 mmHg, no pericardial effusion was seen, and no valvular vegetations were present. After this procedure, the patient was noted to be hypotensive (systolic blood pressure= 65 mmHg) and tachycardic, but afebrile; he was treated with intubation and aggressive fluid resuscitation and transfusion was begun. Frontal chest radiography (Figure 3) was performed.
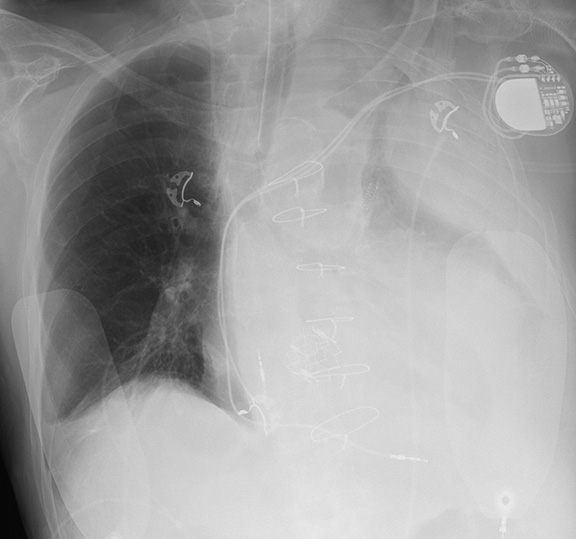
Figure 3. Frontal chest radiography.
Which of the following statements regarding the chest radiograph is most accurate? (Click on the correct answer to proceed to the third of eight pages)