

Correct!
4. Tricuspid valve endocarditis
The apical four chamber view was relatively unrevealing considering the size of the vegetation on the tricuspid valve. However, the RV inflow view demonstrated a large mobile vegetation on the anterior leaflet of the tricuspid valve (> 1.5cm) and involvement of the other leaflets as well. This underscores the importance of obtaining multiple views of each valve when entertaining a diagnosis of endocarditis. The RV inflow view is more typically an advanced echocardiography view. This patient’s view is labeled below in Figure 3.
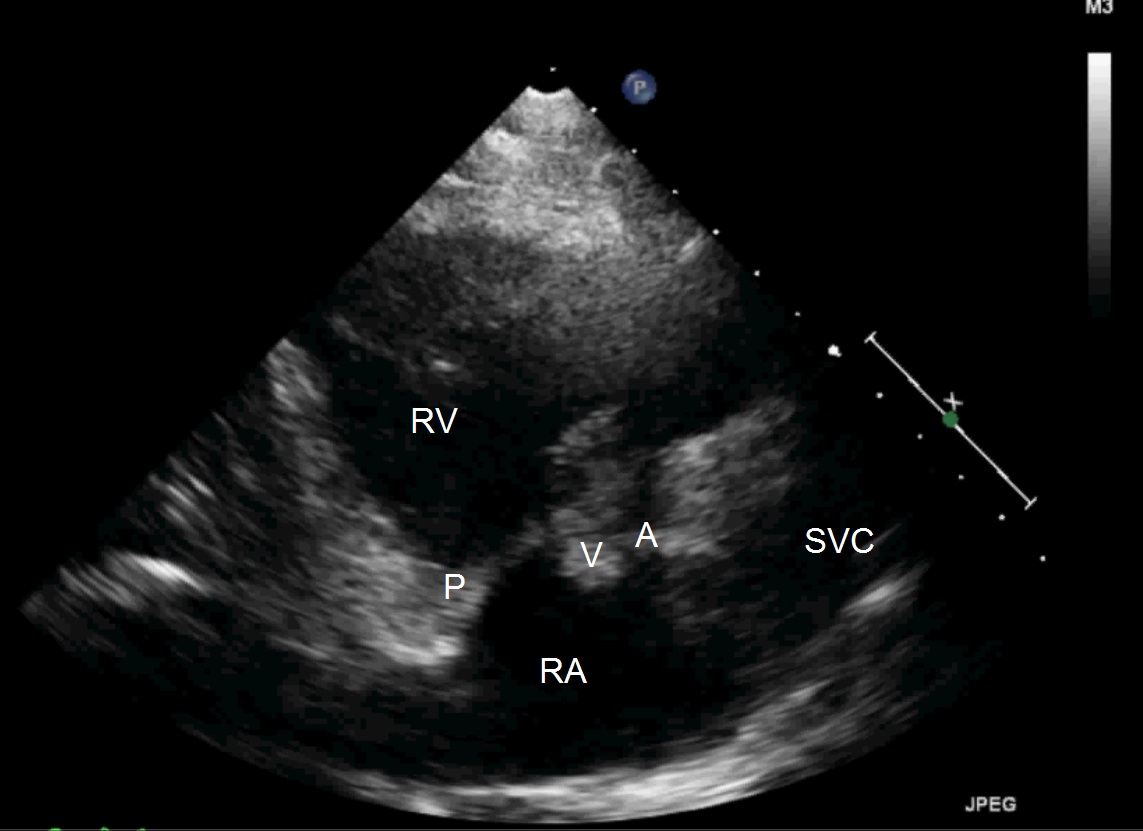
Figure 3. RV inflow of the patient demonstrating vegetation. RV = right ventricle, RA = right Atrium, A = anterior leaflet of tricuspid valve, P = posterior leaflet of tricuspid valve, V = vegetation, SVC =superior vena cava.
A recent prospective cohort study of infective endocarditis patients showed patients with small to moderate pericardial effusions (<10-20 mm) had a greater prevalence of intravenous drug use and more frequent right-sided infective endocarditis than patients without a pericardial effusion. Patients with large to very large effusions, defined as >20 mm or with hemodynamic compromise, had increased 1-year mortality compared patients without an effusion or with a small to moderate sized effusion (1).
Multifocal cavitary lesions with adjacent consolidation were present in the lungs indicating septic emboli was the likely diagnosis for the pneumonia.
A review of the literature explains that - vegetation formation is incited following colonization of a platelet-fibrin aggregate. The pathogenesis of these vegetations in fact does depend on the organism. In this case methicillin susceptible Staphylococcus aureus, which is the typical organism 70% of the time when bacterial endocarditis was present. Streptococci and less commonly Pseudomona and Candida parapsilosis also causes such vegetations. Microbial growth following aggregation activates endothelial cell expression of further fibronectin deposition. This process in turn leads to the vegetation itself and bacterial growth occurs within the fibrin matrix making immune response difficult; thus requiring antibiotic and sometimes surgical intervention to prevent further septic embolization (2,3).
The pathogenic mechanism that explains the increased prevalence of right sided infective endocarditis in intravenous drug users is not fully elucidated. Damage to the right sided valve from injected particulate matter in the setting of injected bacterial load is thought to be important and immune function abnormality may have role in pathogenesis (4).
Nicholas Villalobos MD, Karl Stoltze, Mona Azeem MD
Division of Pulmonary, Critical Care and Sleep Medicine,
University of New Mexico School of Medicine
Albuquerque, NM USA
References