Kenneth Sakata, MD
Richard A. Helmers, MD
Department of Pulmonary Medicine
Mayo Clinic Arizona
Scottsdale, AZ
History of Present Illness
A 69 year old man was admitted to the intensive care unit with shortness of breath and atrial fibrillation with a rapid ventricular response.
PMH, FH, SH
He has a history of peripheral vascular disease, end-stage renal disease and is receiving chronic hemodialysis.
Physical Examination
Afebrile. Pulse 135 and irregular. BP 105/65 mm Hg. SpO2 96% while receiving oxygen at 2L/min by nasal cannula.
HEENT: Unremarkable.
Neck: Jugular venous distention to the angle of the jaw while the head is elevated at 45 degrees.
Lungs: Decreased breath sounds at the right base.
Cardiovascular: Irregularly, irregular rhythm. 2-3+ pretibial edema.
Abdomen: no hepatosplenomegaly.
Radiography
The admission chest x-ray is shown in figure 1.
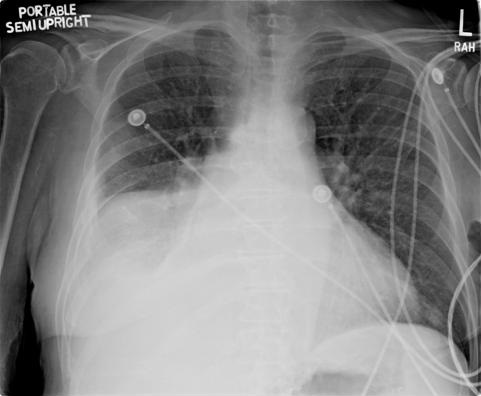
Figure 1. Admission portable chest x-ray.
Which of the following is the best interpretation of the chest x-ray given the clinical situation? (Click on the correct answer to move to the next panel)
- Hepatomegaly elevating the right diaphragm
- Large right pleural effusion
- Paralyzed right diaphragm
- Right lower lobe pneumonia
- Right middle lobe pneumonia
Reference as: Sakata K, Helmers RA. April 2014 critical care case of the month: too much, too fast. Southwest J Pulm Crit Care. 2014;8(4):205-12. doi: http://dx.doi.org/10.13175/swjpcc031-14 PDF