 Figure 1. Video of CT angiography abdomen/pelvis, played caudal to cranial, obtained during assessment in the ED demonstrating obstructive uropathy with bilateral multiloculated urinomas leading to compression of the inferior vena cava. To view Figure 1 video in a separate, enlarged window click here.
Figure 1. Video of CT angiography abdomen/pelvis, played caudal to cranial, obtained during assessment in the ED demonstrating obstructive uropathy with bilateral multiloculated urinomas leading to compression of the inferior vena cava. To view Figure 1 video in a separate, enlarged window click here.
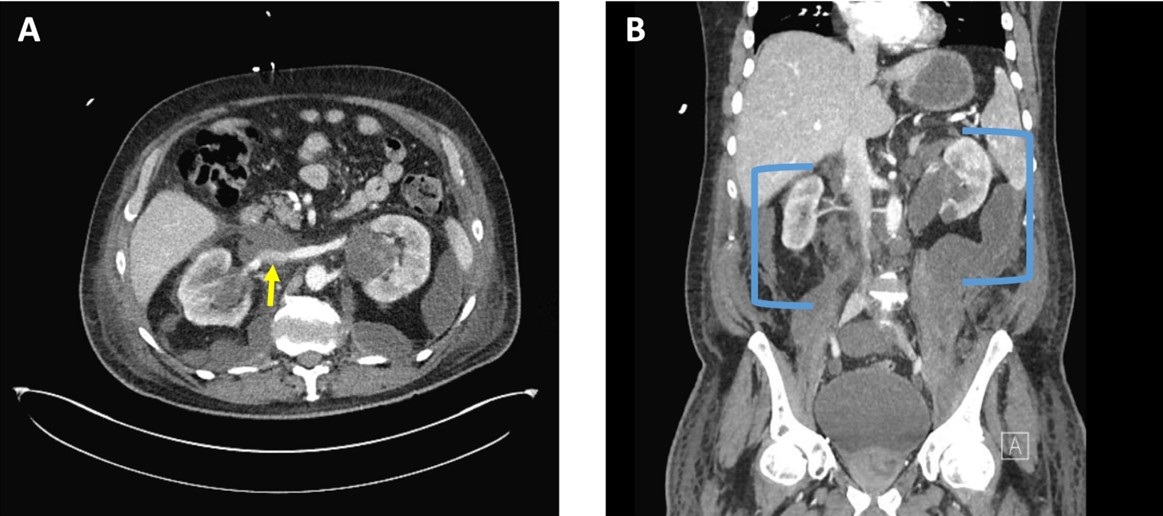 Figure 2. A: CT angiography of the abdomen, axial plane, at the level of the renal veins demonstrating compression of the inferior vena cava (yellow arrow). B: CT angiography of the abdomen and pelvis, coronal plane, demonstrating bilateral multiloculated urinomas (blue brackets). To view Figure 2 in a separate, enlarged window click here.
Figure 2. A: CT angiography of the abdomen, axial plane, at the level of the renal veins demonstrating compression of the inferior vena cava (yellow arrow). B: CT angiography of the abdomen and pelvis, coronal plane, demonstrating bilateral multiloculated urinomas (blue brackets). To view Figure 2 in a separate, enlarged window click here.
A 71-year-old veteran presented to the emergency department with two-weeks of progressive back pain radiating to the abdomen associated low-grade fever, nausea, and new lower extremity edema. The family reported confusion. His medical history was significant for chronic prostatitis and low-grade prostate cancer on biopsy that was lost to follow-up eleven years ago. His only reported medications were aspirin 81 mg daily and naproxen 500mg up to four times a day for his pain.
Vitals were significant for a temperature of 36.1 C, initial blood pressure of 201/74, heart rate of 128/min, respirations at 18/min with a saturation of 97% on 2L NC. Physical exam demonstrated no difference in blood pressures between arms. No abnormal heart sounds. Clear breath sounds to auscultation bilaterally. Flank tenderness to percussion and significant abdominal tenderness over the epigastric and suprapubic region with 3+ pitting edema of the bilateral lower extremities. Screening labs were notable for critical values of a WBC of 43.5 K/mL and potassium of 7 mEq/L with a creatinine of 6.5 mg/dL. He was started on esmolol and hyperkalemia temporizing therapy with the decision made to obtain an urgent contrast enhanced computed tomography of the chest, abdomen, and pelvis.
Imaging confirmed a diagnosis of severe obstructive uropathy with heterogenous prostate with nonspecific small hypodensities, marked bladder distension, hydronephroureter with ureteral wall prominence, and bilateral perinephric multiloculated fluid collections with extension into the abdominal and retroperitoneal spaces leading to indentation of the inferior vena cava (Figures 1 and 2). A Foley catheter was urgently placed with 2.5L of urine immediately relieved and prompt response in blood pressure to 130/80, and resolution of pain, altered mentation, and nausea. He was started on vancomycin and piperacillin/tazobactam for empiric coverage with three percutaneous drains subsequently placed in the multiloculated fluid collections with purulent discharge expressed. Cultures of the output demonstrated no growth. His post-obstructive diuresis was managed with replacement Lactated Ringers’ solution at 75% of the rate of Foley output. He demonstrated complete improvement in leg swelling, heart rate, and WBC and creatinine normalized to 1.1 mg/dL with discharge to home in seven days with close urology follow-up for his prostatic abnormality.
This case of obstructive uropathy extremis, probable cystocerebral syndrome (hypertension, altered mental status, and bladder distension in the elderly), and bilateral urinomas leading to inferior vena cava syndrome is unique to the literature (1). The rupture of the renal fornices, the most delicate and purported “pressure check valve” of the renal conduits, can precipitate the formation of localized urinomas within the perinephric and retroperitoneal space, most commonly unilateral from ureteral or kidney stones or tumor related obstruction, rarely bilateral from bladder outlet obstruction (2). These urinomas, as seen in this case can exert a progressively escalating pressure on the contiguous inferior vena cava, which has been described as “inferior vena cava syndrome” (3). The implications of this pressure increase are manifold, encompassing the observed clinical manifestations ranging from lower extremity edema, worsening kidney perfusion, to hemodynamic instability (3). Management centers upon decompression of the obstruction, treatment of secondary infection with source control, and compensation for post-obstructive diuresis with generally favorable prognosis if recognized early in the clinical course.
Nathan Walton MD1, Elizabeth Mata MD1, Max Hart MD1, Matthew Borchart MD2and Adnan Abbasi MBBS3
1Internal Medicine Program, University of Arizona College of Medicine – Tucson
2Department of Medicine, Pulmonary & Critical Care, University of Arizona College of Medicine – Tucson
3Department of Medicine, Pulmonary & Critical Care, Southern Arizona Veterans Affairs Health Care System (SAVAHCS) – Tucson
References
- Blackburn T, Dunn M. Cystocerebral syndrome. Acute urinary retention presenting as confusion in elderly patients. Arch Intern Med. 1990 Dec;150(12):2577-8. [CrossRef][PubMed]
- Gershman B, Kulkarni N, Sahani DV, Eisner BH. Causes of renal forniceal rupture. BJU Int. 2011 Dec;108(11):1909-11; discussion 1912. [CrossRef][PubMed]
- Lawrensia S, Khan YS. Inferior Vena Cava Syndrome. 2023 May 20. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan–. [PubMed]