Ramzi Ibrahim MD, João Paulo Ferreira MD
Department of Medicine, University of Arizona – Tucson and Banner University Medical Center
Tucson AZ USA
Abstract
Pulmonary emboli are associated with high morbidity and mortality, prompting early diagnostic and therapeutic considerations. Utilization of rapid point-of-care ultrasound (POCUS) to assess for signs of pulmonary emboli can provide valuable information to support immediate treatment. We present a case of suspected pulmonary embolism in the setting of pharmacological prophylaxis for venous thromboembolism with identification of right heart strain on bedside POCUS exam. Early treatment with anticoagulation was initiated considering the clinical presentation and POCUS findings. CT angiogram of the chest revealed bilateral pulmonary emboli, confirming our suspicion. Utilizing POCUS in a case of suspected pulmonary emboli can aid in clinical decision making.
Case Presentation
Our patient is a 50-year-old man with a history of morbid obesity, obstructive sleep apnea, and poorly controlled diabetes mellitus type 2 who was admitted to the hospital for sepsis secondary to left foot cellulitis and found to have left foot osteomyelitis with necrosis of the calcaneus. The patient was started on intravenous antimicrobials, underwent incision and debridement, and completed a partial calcanectomy of the left foot. During the hospital course, he remained on subcutaneous unfractionated heparin at 7,500 units three times a day for prevention of deep vein thrombosis. On post-operative day 12, he developed acute onset of dyspnea requiring 2 liters of supplemental oxygen and was slightly tachycardic in the low 100s. He complained of chest tightness without pain, however, he denied lower extremity discomfort, palpitations, orthopnea, or diaphoresis. Electrocardiogram was remarkable for sinus tachycardia without significant ST changes, T-wave inversions, conduction defects, or QTc prolongation. Rapid point-of-care ultrasound (POCUS) at bedside revealed interventricular septal bowing, hypokinesia of the mid free right ventricular wall, and increased right ventricle to left ventricle size ratio (>1:1 respectively) (Figures 1 and 2).
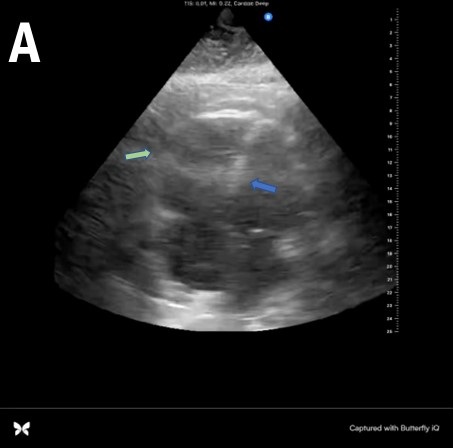
 Figure 1. A: Static apical 4-chamber view showing interventricular bowing into the left ventricle (blue arrow), significantly enlarged right ventricle, and right ventricular free wall hypokinesia (green arrow). B: Video of apical 4-chamber view.
Figure 1. A: Static apical 4-chamber view showing interventricular bowing into the left ventricle (blue arrow), significantly enlarged right ventricle, and right ventricular free wall hypokinesia (green arrow). B: Video of apical 4-chamber view.
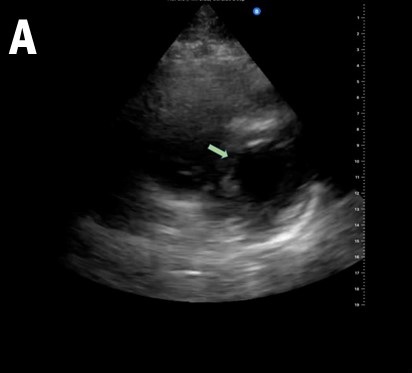
 Figure 2. A: Static parasternal short axis view showing interventricular septal bowing in the left ventricle (green arrow). B: Video of parasternal short axis view.
Figure 2. A: Static parasternal short axis view showing interventricular septal bowing in the left ventricle (green arrow). B: Video of parasternal short axis view.
With these findings, the patient was started on therapeutic anticoagulation. CT angiogram of the chest revealed a large burden of bilateral pulmonary emboli (PE). The pulmonary embolism severity index (PESI) score was 130 points which is associated with a 10%-24.5% mortality rate in the following 30 days. Formal echocardiogram showed a severely dilated right ventricle with reduced systolic function, paradoxical septal movement, and a D-shaped left ventricle. Patient remained hemodynamically stable and was discharged home after transition from heparin to rivaroxaban.
Discussion
Pulmonary emboli remain a commonly encountered pathological phenomenon in the hospital setting with a mortality rate ranging from <5% to 50% (1). Venous thromboembolism prophylaxis has been shown to reduce the risk of VTE in hospitalized patients, however, this does not eliminate the risk completely. Prompt diagnosis allows earlier treatment and improved outcomes however this is often challenging given the lack of specificity associated with its characteristic clinical symptoms (2). In the proper context, utilization of POCUS can aid the diagnosis of PE by assessing for signs of right ventricular strain. Characteristic findings seen on a cardiac-focused POCUS that represent right ventricular strain include McConnell’s sign (defined as right ventricular free wall akinesis/hypokinesis with sparing of the apex), septal flattening, right ventricular enlargement, tricuspid regurgitation, and tricuspid annular plane systolic excursion under 1.6 cm (3). Their respective sensitivities and specificities are highly dependent on the pre-test probability. For example, a prospective cohort study completed by Daley et al. (4) in 2019 showed that for patients with a clinical suspicion of PE, sensitivity of right ventricular strain was 100% for a PE in patients with a heart rate (HR) >110 beats per minute, and a sensitivity of 92% if HR >100 BPM. This study provides evidence to support the use of cardiac focused POCUS in ruling out pulmonary emboli in patients with signs of right ventricular strain and abnormal hemodynamic parameters such as tachycardia. Additionally, in settings where hemodynamic instability is present and the patient cannot be taken to the CT scanner for fear of decompensation, rapid POCUS assessment can be helpful. In our patient, given the acute need for supplemental oxygenation and dyspnea, along with his risk factors for a thromboembolic event, the use of POCUS aided in our clinical decision making. The yield of information that can be provided by POCUS is vital for early diagnostic and therapeutic decision making for patients with a clinical suspicion of pulmonary emboli.
References
- Torbicki A, Perrier A, Konstantinides S, et al. Guidelines on the diagnosis and management of acute pulmonary embolism: the Task Force for the Diagnosis and Management of Acute Pulmonary Embolism of the European Society of Cardiology (ESC). Eur Heart J. 2008 Sep;29(18):2276-315. [CrossRef][PubMed]
- Roy PM, Meyer G, Vielle B, et al. Appropriateness of diagnostic management and outcomes of suspected pulmonary embolism. Ann Intern Med. 2006 Feb 7;144(3):157-64. [CrossRef][PubMed]
- Alerhand S, Sundaram T, Gottlieb M. What are the echocardiographic findings of acute right ventricular strain that suggest pulmonary embolism? Anaesth Crit Care Pain Med. 2021 Apr;40(2):100852. [CrossRef] [PubMed]
- Daley JI, Dwyer KH, Grunwald Z, et al. Increased Sensitivity of Focused Cardiac Ultrasound for Pulmonary Embolism in Emergency Department Patients With Abnormal Vital Signs. Acad Emerg Med. 2019 Nov;26(11):1211-1220. [CrossRef][PubMed]
Cite as: Ibrahim R, Ferreira JP. Point-of-Care Ultrasound and Right Ventricular Strain: Utility in the Diagnosis of Pulmonary Embolism. Southwest J Pulm Crit Care Sleep. 2022;25(2):34-36. doi: https://doi.org/10.13175/swjpccs040-22 PDF