G. Zacharia Reagle DO
Eyad Almasri MD
Stuart J. Maxwell MD
Departments of Internal Medicine, Division of
Pulmonary and Critical Care
and Emergency Medicine
UCSF Fresno
Fresno, CA
History of Present Illness:
A 63 year-old man was brought to the emergency department (ED) with a report of acute onset of dyspnea. The dyspnea had started at rest less than one hour prior to ED presentation. It quickly progressed to severe respiratory distress. His initial vital signs were recorded as a BP of 124/69, pulse of 112, respiratory rate of 26 with an oxygen saturation (SpO2) of 88% on 15 liters per minute (lpm) of oxygen via a non-rebreather mask. He was placed on non-invasive ventilation with intermittent episodes of brief desaturation into the 60% range. He was subsequently intubated without incident. Immediately following intubation he experienced a pulseless electrical activity (PEA) cardiopulmonary arrest.
Past Medical History:
- Diabetes mellitus
- Coronary Artery Disease
- Hypertension
- Deep Venous Thrombosis
Past Surgical History:
- Coronary Artery Bypass Graft – 2 vessel
Medications:
-
Atorvastatin 40mg PO daily
-
Insulin glargine 10u SQ daily
-
Lisinopril 10mg PO daily
- Warfarin – had been stopped due to difficulty with compliance.
Social History:
- Married
- Owns and manages a series of used car lots.
- Lifetime non-smoker
- Reports a remote history of chronic alcohol use, but quit in 2005 when he was diagnosed with coronary artery disease.
- He denied illicit drug use.
Physical Exam:
General: Intubated, on a fentanyl infusion at 50mcg per hour.
Vitals: BP: 122/63 HR: 123 RR: 24 T: 35.6
HEENT: NC/AT, PERRL, neck supple without JVD noted.
Lungs: equal chest expansion was noted with clear lung sounds.
Heart: Tachycardic and regular with a good S1 and S2, no murmurs or gallops were appreciated.
Abdomen: soft, obese, good bowel sounds.
Extremities: cold to the touch with no edema, or clubbing.
Neurological: Nonfocal exam with suppressed Glasgow Coma Scale after sedation for intubation.
Skin: No rashes noted.
Laboratory:
Complete Blood Count (CBC): White blood cell count (WBC) 8.8 x 1000 cells/µL, hemoglobin 14.6 g/dL, hematocrit 43.7, platelets 191,000 cells/µL
Chemistry: Sodium 139 meq/L, potassium 3.6 meq/L, chloride 106 meq/L, bicarbonate (CO2) 19 meq/L, blood urea nitrogen (BUN) 20 mg/dL, creatinine 0.7 mg/dL, glucose 459 mg/dL, magnesium 2.0 meq/L, phosphorus 3.4 mg/dL
Liver Function Tests: Albumin 4.1 g/dL, ALP 59 U/L, AST 30 U/L ALT 31 U/L. total bilirubin 0.4 mg/dL
Coagulation: Prothrombin time 13.9 seconds, INR 1.1, activated partial thromboplastin time (aPTT) 24.2 seconds
Troponin: 0.007 ng/ml
Brain naturetic peptide (BNP): 39 pg/ml
Arterial Blood Gases (ABG): pH 7.27, pCO2 38, pO2 38
Imaging:
The patient was immediately taken for a chest CT pulmonary angiogram. As he was on the CT scan table, the CT technician discovered that his IV line was malfunctioning. Before the line could be replaced, he had several non-contrast chest CT cuts obtained (Figure 1).
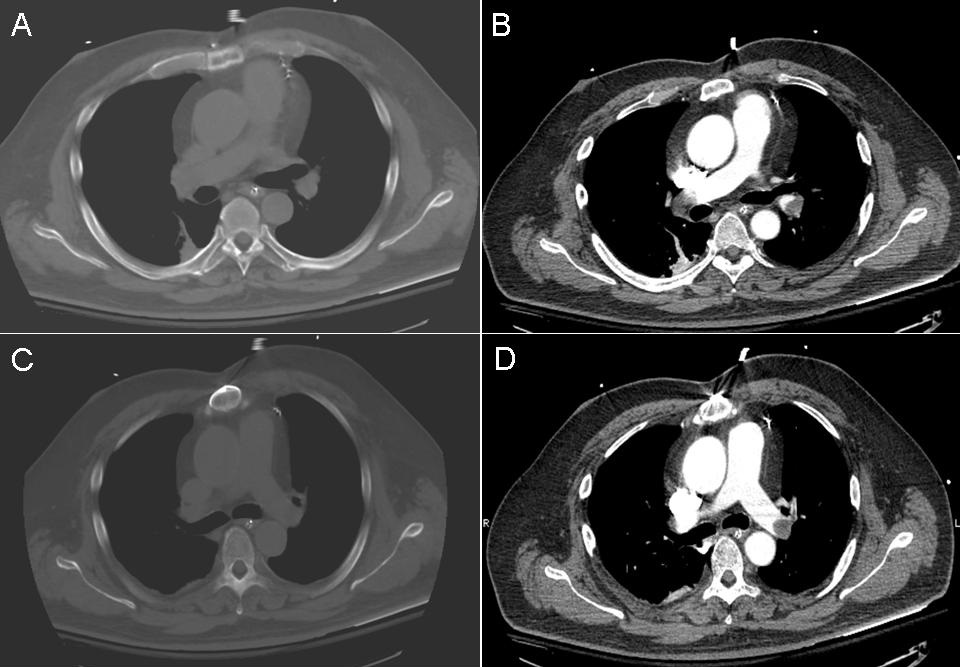
Figure 1. Images A & C are non-contrast cuts while images B & D are comparison cuts that became available after the contrast study was obtained.
How often are intravascular filling defects seen on non-contrast chest CT images and what is the positive predictive value (PPV) of non-contrast images for pulmonary embolism (PE)? (Click on the correct answer to proceed to the next panel)
- Filling defects are often seen on non-contrast CT images and are diagnostic for pulmonary embolism.
- Filling defects can be seen on non-contrast images but have a low PPV.
- Filling defects indicating pulmonary embolism are never seen on non-contrast images.
- Filling defects indicating pulmonary embolism are sometimes seen on non-contrast images and have a high PPV for PE.
Reference as: Reagle GZ, Almasri E, Maxwell SJ. October 2014 pulmonary case of the month: a big clot. Southwest J Pulm Crit Care. 2014;9(4):199-207. doi: http://dx.doi.org/10.13175/swjpcc118-14 PDF