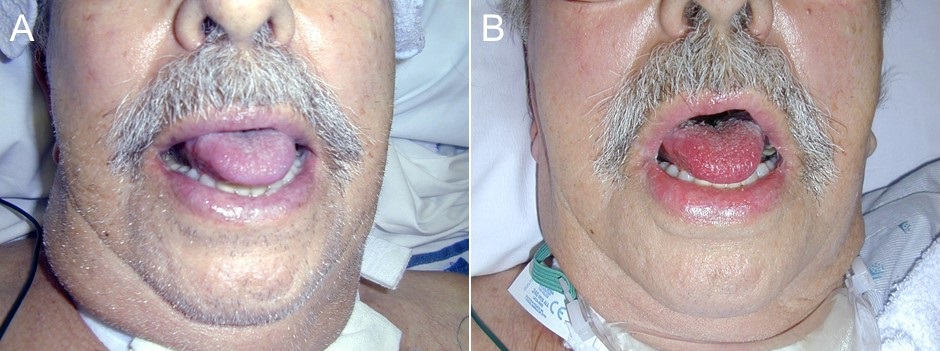
Figure 1. A: cyanotic lips and tongue. B: restoration of reddish color after methylene blue infusion.

Figure 2. Patient’s blood showing a chocolate brown color.
A 62-year-old man with a sternal infection post-coronary artery bypass grafting was transferred because of increasing oxygen requirements, decreased mental status and Candida paralopsis fungemia. He had been treated with multiple antibiotics including sulfonamides and had eventually undergone a tracheostomy. Cetacaine was used for complaints of a sore throat. Physical examination showed cyanotic lips and tongue (Figure 1A). Blood drawn was a chocolate brown color (Figure 2). His SpO2 was 88%, however, arterial blood gases showed his SaO2 was 100% and his PaO2 453 mmHg. Co-oximetry showed 26% methemoglobin. He was administered 0.2mL/kg of 1% solution of methylene blue and his cyanosis rapidly cleared (Figure 1B).
Methemoglobinemia is a condition characterized by increased quantities of hemoglobin with iron oxidized to the ferric (Fe3+) form (1). Methemoglobin is useless as an oxygen carrier and thus causes a varying degree of cyanosis and hypoxia. It can be genetic but is usually caused by exposure to drugs or toxins. Symptoms are proportional to the fraction of methemoglobin. A normal methemoglobin fraction is about 1%. Symptoms associated with higher levels of methemoglobin are: 3-15% - cyanosis; 25-50% - headache, dyspnea; 50-70% - cardiac arrhythmias, altered mental status, delirium, seizures, coma; >70% - death. Drugs most commonly associated with methemoglobinemia include topical and injected local anesthetics (benzocaine, lidocaine, cetacaine), sulfonamides (dapsone), and nitrates (nitroprusside).
Intravenous methylene blue, a reducing agent, is the traditional antidotal agent (1). Exchange transfusion and hyperbaric oxygen treatment are second-line options for patients with severe methemoglobinemia who do not respond to methylene blue or who cannot be treated with methylene blue (e.g., those with glucose-6-phosphate dehydrogenase [G6PD] deficiency).
Robert A. Raschke, MD, MS
University of Arizona College of Medicine-Phoenix and Banner University Medical Center
Phoenix, AZ USA
Reference
- Denshaw-Burke M. Methemoglobinemia. Medscape. Nov 14, 2017. Available at: https://emedicine.medscape.com/article/204178-overview (accessed 1/11/18).
Cite as: Raschke RA. Medical image of the week: methemoglobinemia. Southwest J Pulm Crit Care. 2018;16(1):49-50. doi: https://doi.org/10.13175/swjpcc007-18 PDF