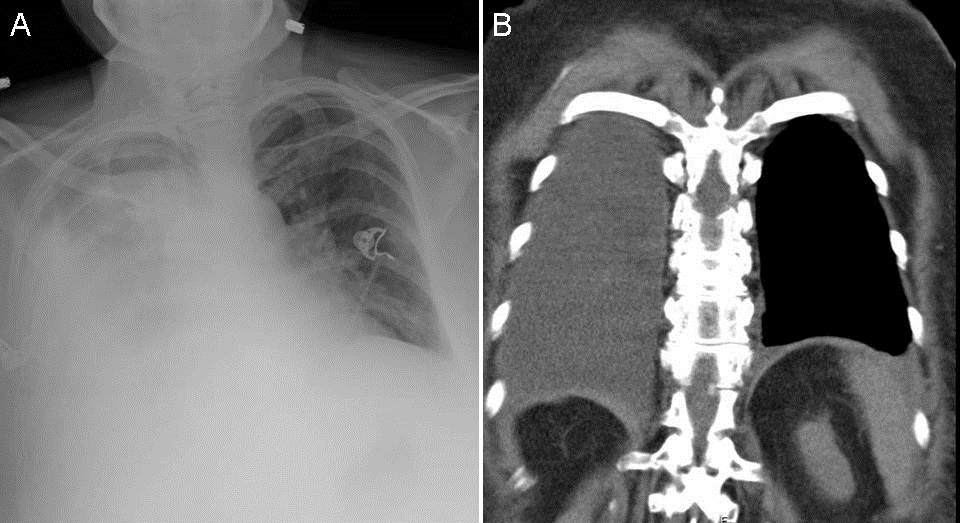
Figure 1. Panel A: Chest x-ray showing right pleural effusion. Panel B: Coronal view of the thoracic CT scan in soft tissue windows showing right pleural effusion.
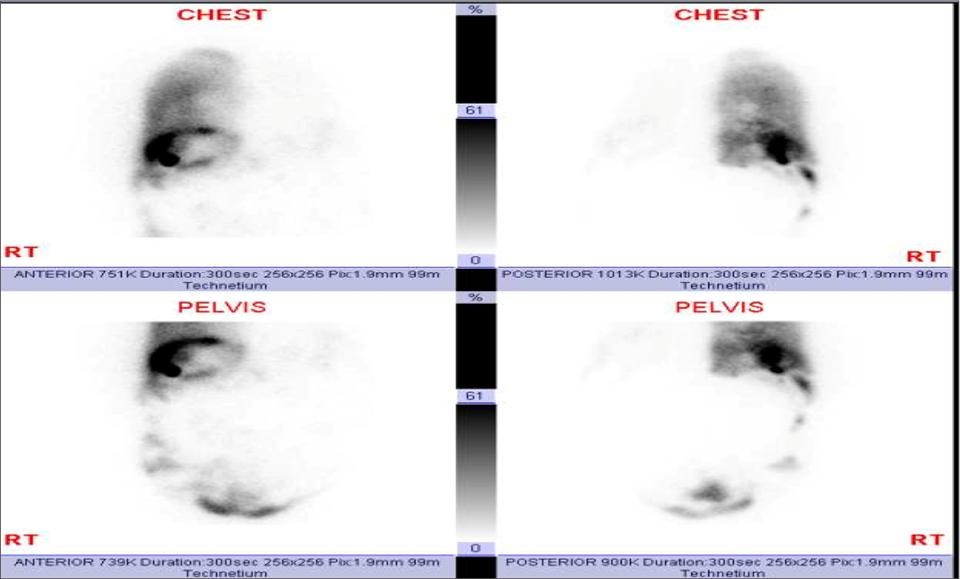
Figure 2. Nuclear scan after intraperitoneal injection of technetium 99mTc albumin aggregated (99mTc-MAA). After less than one hour most of the tracer migrated into the right hemithorax consistent with hepatic hydrothorax.
A 63 year-old woman, with known alcoholic liver cirrhosis, esophageal varices with history of banding presented to an outside hospital with progressive shortness of breath, and was found to have a large right transudative pleural effusion. The patient underwent 2 diagnostic and therapeutic thoracenteses within 3 days, removing 1100 ml and 1500 ml respectively. No ascites was present. At the time of admission the patient had recurrent right effusion (Figure 1). Abdominal ultrasound showed minimal free intrabdominal fluid and she had signs of third spacing on her lower extremities. The patient underwent intraperitoneal injection of Technetium 99mTc albumin aggregated (99mTc-MAA). After less than one hour most of the tracer migrated into the right hemithorax consistent with hepatic hydrothorax (Figure 2).
While the exact mechanism involved in the development of hepatic hydrothorax is incompletely understood, it probably results from the passage of ascitic fluid from the peritoneal into the pleural cavity through small diaphragmatic defects. These are typically < 1 cm (and may be microscopic) and are generally located in the tendinous portion of the diaphragm. The negative intrathoracic pressure generated during inspiration favors the passage of the fluid into the pleural space. Thus, patients may have only mild or clinically undetectable ascites.
Once the diagnosis is made treatment follows algorithms for treatment of refractory ascites and include salt and water restriction, diuretics, and other validated options for portal hypertension. Repeated thoracentesis and chest tube placement is discouraged.
Huthayfa Ateeli, Justin Lee, Irbaz Riaz, Meenal Misal
Department of Internal Medicine
University of Arizona
Tucson, AZ
References
-
Huang PM, Chang YL,Yang CY,Lee YC.The morphology of diaphragmatic defects in hepatic hydrothorax: thoracoscopic finding. J Thorac Cardiovasc Surg. 2005;130:141-5. [CrossRef] [PubMed]
-
Lieberman FL, Hidemura R, Peters RL, Reynolds TB. Pathogenesis and treatment of hydrothorax complicating cirrhosis with ascites. Ann Intern Med. 1966;64:341-51. [CrossRef] [PubMed]
-
Emerson PA, Davies JH. Hydrothorax complicating ascites. Lancet. 1955; 268:487-8. [CrossRef] [PubMed]
-
Mouroux J, Perrin C, Venissac N, Blaive B, Richelme H. Management of pleural effusion of cirrhotic origin. Chest. 1996;109:1093-6. [CrossRef] [PubMed]
-
Chen A, Ho YS, Tu YC, Tang HS, Cheng TC. Diaphragmatic defect as a cause of massive hydrothorax in cirrhosis of liver. J Clin Gastroenterol. 1988;10:663-6. [CrossRef] [PubMed]
Reference as: Ateeli H, Lee J, Riaz I, Misal M. Medical image of the week: hepatic hydrothorax. Southwest J Pulm Crit Care. 2015;10(1):47-8. doi: http://dx.doi.org/10.13175/swjpcc004-15 PDF