University of Arizona College of Medicine-Phoenix
Phoenix, AZ USA
History of Present Illness:
A 75-year-old man presented from a skilled nursing facility with altered mental status and hypotension. He had a seven-year-long history of steroid-dependent myasthenia gravis, but had previously declined Covid vaccination, and subsequently experienced a severe case of COVID-19 pneumonia five months prior to admission. This resulted in chronic respiratory failure and renal failure for which he subsequently underwent tracheostomy, tunneled subclavian vein dialysis catheter placement and percutaneous endoscopic gastrostomy (PEG). He had resided in a skilled nursing facility since then, requiring four subsequent hospital readmissions for complications. These sequentially included septic shock due to a catheter associated blood stream infection, an intra-abdominal abscess due to PEG migration into the peritoneum resulting in fungal blood stream infection, recurrent intra-abdominal infection with multiple organisms, and bacterial pneumonia. Treatment of these infectious complications included replacement of the tunneled dialysis catheter and exploratory laparotomy with debridement of multiple abscesses. The abdominal wound was left open to heal by secondary intention. The patient received multiple courses of broad-spectrum antibiotics over the preceding four months including (at various times) ampicillin/sulbactam, anidulafungin, piperacillin/tazobactam, cefepime, colistin, meropenem, micafungin, TMP/SMZ, and tobramycin. During his most recent admission three weeks previously, the patient experienced rectal hemorrhage due to ulceration caused by a rectal tube, and a sacral decubitus pressure ulcer was discovered.
Late on the day of admission, staff at the skilled nursing facility where the patient resided noted altered mental status and a BP of 55/38, but reported no other new symptoms. They administered 2L of normal saline, cefepime and vancomycin, and transferred the patient for admission to our ICU at l am. The patient was non-verbal due to delirium and ventilator dependence and could offer no further history. His full code status was described by skilled nursing staff as “adamantly full code.”
Physical examination:
- Vital Signs: Temperature: 96.5 F. Heart rate 114 bpm. Respiratory rate 19 bpm. Blood pressure BP 74/36 mmHg (on norepinephrine 50 mcg/min infusion). SpO2 100% (on 30% FiO2).
- The patient was chronically critically-ill appearing and severely deconditioned.
- An 8.0 cuffed tracheostomy, a PEG and a tunneled right subclavian hemodialysis catheter were present– none of which appeared obviously infected.
- HEENT was otherwise unremarkable (ophthalmological examination was not performed).
- The lungs were clear.
- Cardiac exam was tachycardic and hyperdynamic.
- The abdomen had a large midline wound lined with pink, non-odorous granulation tissue. The abdomen was otherwise soft and nontender.
- A 6X6cm sacral pressure wound extended into subcutaneous tissues and was not obviously infected.
- Stools removed from a rectal tube were maroon and heme positive.
- No skin lesions were noted.
Laboratory results:
- CBC: WBCC 24.4 x 109/L, Hb 8.3 g/dL, platelets 193 x 109/L
- Electrolytes: Na 142 mmol/L, K 3.7 mEq/L mEq/L, Cl 109, bicarb 11 mEq/L,
- Renal function: BUN 94 mg/dL, creatinine 3.5 mg/dL
- Liver Enzymes: AST 1790 U/L, ALT 1111 U/L, Alkaline phosphatase 270 IU/L, albumin 1.8 mg/dL, t-bilirubin 0.7 mg/dL
- Lactate 6.4 mmol/L
- Procalcitonin 12.7 ng/mL
- Random cortisol level was 8.2 mcg/dL.
A chest radiogram is depicted below (Figure 1).
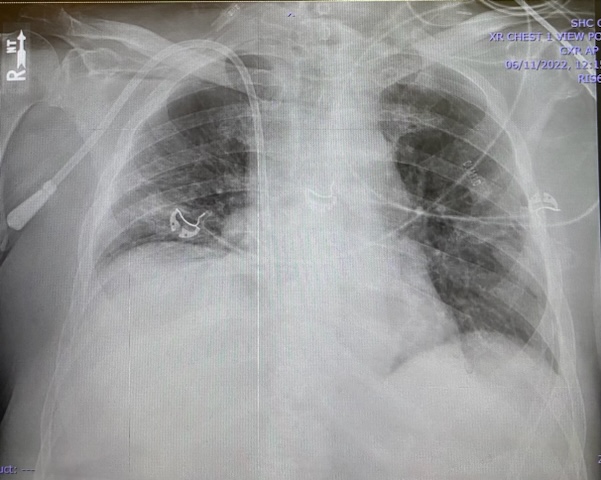
Figure 1. Admission portable chest x-ray.
A presumptive diagnosis of septic shock and adrenal insufficiency were made, and piperacillin/ tazobactam, vancomycin and hydrocortisone were administered intravenously. The patient received an additional 3.5L of normal saline over the following 8 hours; but nevertheless, required increasing doses of intravenous norepinephrine, phenylephrine, vasopressin and epinephrine infusions to maintain MAP >60 mmHg. It is now morning.
Which of the following actions are most important to be immediately undertaken? (Click on the correct answer to be directed to the second of 4 pages)
- The tunneled dialysis catheter should be removed.
- Computerized tomography of the chest, abdomen and pelvis should be obtained.
- Prior microbiology results and local antibiograms should be reviewed.
- Antibiotic coverage should be broadened.
- Point of Care echocardiography should be performed.